Having carotid artery disease raises your risk of ischemic stroke, which is a stroke due to a blocked blood vessel in the brain.
What is carotid artery disease?
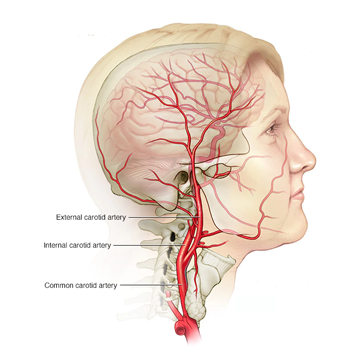
The carotid arteries are the main blood vessels supplying the front part of the brain. In carotid artery disease, one or both of the carotid arteries becomes narrowed inside, as well as becoming stiffer. This makes it harder for blood to flow, and makes clots more likely to form.
Arteries can become narrower inside if they get clogged with fatty substances in the blood sticking to the lining of the artery walls. These substances include cholesterol and other fats, which combine with other materials like blood cell fragments. This can build up to form thickened areas, also known as plaques, on the artery wall. This is also known as atheroma, or atherosclerosis.
As we age, our arteries gradually become stiffer and thicker. Having a build-up of atheroma inside the arteries speeds up this process, making the artery narrower inside (also known as stenosis). This can alter blood flow, and make clots more likely to form.
Clot fragments can then break off and go up to the brain, to block a blood vessel inside the brain and cause a stroke. Sometimes a clot can block the artery itself, cutting off the blood supply at this point. This process is called thrombosis.
How can carotid artery disease cause a stroke or TIA?
A stroke is a brain attack. It happens when the blood supply to part of the brain is cut off, killing brain cells. Someone with carotid artery disease is more likely to have a stroke due to a blockage or clot in the brain, also known as an ischaemic stroke. Carotid artery disease can lead to stroke in two ways.
- Total blockage (occlusion):Occlusion is the medical term for when a plaque (atheroma) completely blocks a carotid artery, cutting off the blood supply to the brain and causing a stroke.
- Clot in the artery (thrombosis):As well as making the arteries narrower (stenosis), atheroma canmake the inner surface of artery walls fragile and likely to break up. If the atheroma ruptures, it exposes the artery lining, and a clot forms over the damaged area.
Who is at risk of carotid artery disease?
Carotid artery disease causes around a quarter of all ischaemic strokes in the UK. While we all develop some narrowing in our arteries as we get older, other factors can make you more likely to develop carotid artery disease. The main risk factors are:
This has three categories of measurement which are:
Minor: less than 50% narrowed
Moderate: 50-69% narrowed
Severe: 70% narrowed or more
How is carotid artery disease diagnosed?
Carotid artery disease is usually diagnosed when you have a stroke. It can also be diagnosed after a transient ischaemic attack (TIA). This is the same as a stroke, but the symptoms last a short amount of time. Occasionally, a doctor might discover that you have some narrowing if you are having tests on these arteries for another health reason.
Your doctor may listen to the sound of your blood flow through your carotid arteries using a stethoscope. A whooshing sound, known as a carotid bruit, can be a sign that there is some narrowing, although this is not very reliable. You will then be referred to a hospital specialist for further tests. A useful test for carotid artery disease is an ultrasound scan (known as a carotid Doppler). It is a completely painless procedure. A small probe is passed over the side of your neck to build up a picture of your arteries. The specialist can then see whether there is any narrowing and, if so, whether it is severe enough to benefit from having an operation.
You will probably have further imaging checks to confirm this diagnosis. These may be computed tomography angiography (CTA) scans or magnetic resonance angiography (MRA) scans, which sometimes need a special dye injection (called a contrast agent). In the UK, the NASCET scale (North American Symptomatic Carotid Endarterectomy Trial) is usually used to measure carotid stenosis.
Carotid endarterectomy may be carried out under local or general anaesthetic in an operation that takes one to two hours. If both of your carotid arteries need surgery, this is usually done in two separate operations.
The surgeon makes a small cut in the side of your neck so they can see your carotid artery, which will then be clamped shut. If need be, a small piece of tubing (shunt) can be used to re-route blood flow along another artery to make sure your brain still gets enough blood.
The surgeon then opens up your artery and removes the inner lining and any fatty deposits (plaques). The artery is closed with stitches, or with a patch. The patch can be made of artificial fibres or be a graft taken from another blood vessel.
The operation usually takes between one and two hours. Most people recover remarkably quickly. Within a few hours you can usually sit up in bed, and are able to go home in a couple of days.
The wound in your neck should heal to a fine scar after a few months. You may be advised to limit your physical activity for a short period. Most people can return to work after three to four weeks but extra care needs to be taken in jobs that involve manual labour. Where possible, light duties should be performed until you fully recover.
You will be able to return to driving two to three weeks following your operation, providing that you can perform an emergency stop safely and look over your shoulder. However, some conditions, including stroke and TIA come with a short or longer term driving ban from the DVLA (or DVA in Northern Ireland).
- re-stenosis, or the carotid arteries becoming blocked Up to 4% of people will need to have further surgery.
As with any major operation, these risks should be explained to you. It is normal to feel anxious or frightened by this so talk to your surgeon and anaesthetist about your concerns.
It is a good idea to prepare for an appointment with specialists by writing down a list of questions in advance. You may like to consider the following:
Questions to ask before the operation
You may want to write down what the specialists tell you and discuss it with friends or family.
How can it be treated?
There are procedures that can reduce the risk of a stroke or TIA, but, they will only be offered to you if your artery has moderate or severe stenosis. This is because the procedures themselves carry risks, and are most successful at reducing stroke risk when stenosis is over 50%. The main procedure is an operation called carotid endarterectomy.
For arteries with minor stenosis, the risks of the operation are considered too high. These arteries are much less likely to cause a stroke and can still supply your brain with enough blood.
Carotid endarterectomy
Carotid endarterectomy is an operation to clear the blockages from inside an artery. It is well-established and is the main procedure used.
If you smoke you will be advised to stop smoking before the operation. Smoking reduces the amount of oxygen in your blood and can increase your risk of breathing problems during the procedure or getting a chest infection.
Ideally, surgery should be carried out within one week of your symptoms of stroke or transient ischaemic attack (TIA).
What are the risks?
As with any operation, there are some risks associated with carotid endarterectomy.
There is about a 2% risk of having a stroke during surgery. This is due to a small blood clot, or other debris, breaking free during the operation and travelling to your brain. So carotid endarterectomy is only recommended if you have a moderate or severe stenosis, where the risk of having another stroke is greater than the risk associated with the procedure. Just under one in a hundred people die, which usually happens when there is stroke or heart attack soon after the operation.
Complications are more likely if you are older, a smoker, or have had a recent stroke. You can also be more at risk of complications if you have a blockage in both carotid arteries, and if you have other health conditions such as heart disease and high blood pressure. Complications can include:
- Wound infection, which affects less than 1% of people, and can be treated with antibiotics
- Bleeding from the site of your wound
- Nerve injury, which affects around 4% of people and is usually This can cause a hoarse voice, weakness, or numbness on one side of your face. These symptoms usually disappear within a month.
- Numbness or slight pain around your wound, which can be treated with painkillers
This procedure is less invasive than the endarterectomy because it does not involve open surgery of the neck. The evidence shows that this procedure is safe and effective, with similar long-term risks of a stroke as carotid endarterectomy.
The procedure is done under local anaesthetic. A small flexible tube is passed into the carotid artery through the femoral artery in your groin. This is done under the guidance of an X-ray of your arteries, and a dye (contrast) will be injected into the tube. The tube has a small balloon at the end of it. When this tube reaches the narrowed area, the balloon is inflated up to around 5mm.
A small wire mesh cylinder called a stent is inserted to keep your artery open, improving blood flow. The stent stays there permanently. This widens your artery, allowing your blood to flow through it again. The balloon is then removed.
After the operation you will need to lie flat and still for an hour or so afterwards to prevent bleeding from the artery. You will stay in hospital overnight and go home the following day.
Carotid artery stent
There is an alternative to the carotid endarterectomy procedure that is called carotid artery stent placement, often known as stenting.
- an allergic reaction or kidney problems
- a blockage or rupture in your carotid artery – this can sometimes be treated with a stent. If this isn’t possible, an operation may be needed to repair your artery.
The advantages of stenting are that it is less invasive, avoids wound complications and has a lower risk of nerve damage. However, clinical trials suggest that the short term risk of minor stroke seems to be higher with stenting than endarterectomy, so stenting is usually offered only when endarterectomy is not recommended.
Speak to your consultant about your options and ask lots of questions until you feel you understand everything. You may wish to ask why you are being offered stenting rather than endarterectomy. There are several possible answers to this question, and they may include the anatomy of your carotid arteries, the experience of the medical staff, or your general health and age.
Carotid artery stent
As with carotid endarterectomy, complications can occur after stenting and the risk of another stroke and death after both procedures are similar. Therefore, as with endarterectomy, it will also only be recommended if you have moderate to severe stenosis. Other rare complications of this procedure include:
- bruising where the tube enters your femoral artery
- bleeding from this point which may require an operation (affects about 1% of all cases)
Other options
If you choose not to have an operation, or if you are unsuitable for an operation, you will be given medicine and lifestyle advice to help to reduce your risk of a further stroke or TIA.
How can I reduce my risk of stroke or TIA?
If you have carotid artery disease, it is particularly important to maintain a healthy lifestyle. This will help to reduce the risk of your arteries becoming blocked up again, and will reduce the risk of a further stroke or TIA.
Doctors will check you for any other health conditions linked to stroke. If you have any of these conditions, you will be treated to lower the risk of another stroke. These include:
- high blood pressure
- atrial fibrillation (irregular heartbeat)
- diabetes
- high cholesterol
You will be offered treatment for any health condition you may have, and one of the best ways to reduce your risk is to carry on with any treatment you are given.
You will be given advice about making healthy lifestyle choices, like losing weight if you need to, and being more active. All of these can help to manage your health conditions, as well as reducing your risk of a stroke. Find out more about active steps everyone can take in our guide L11, How to reduce your risk of a stroke.
